Kirsten Tillisch a doctor of medicine at the University of California in Los Angeles, along with her colleagues recently published the results of their meta-analysis on brain activity studies for patients with Irritable Bowel Syndrome. While reviewing these past studies they found that the brains of patients with Irritable Bowel Syndrome were more likely to experience activity in emotional arousal sectors(pregenual anterior cingulate cortex, amygdala) and endogenous pain modulation sector(midbrain cluster). The overall results of the analysis “support[s] a role for central nervous system dysregulation in IBS.” Continue reading “Irritable Bowel Syndrome Causes Emotion & Pain Sensitivity To Increase” »
The FDA recently granted fast-track status for the drug MuDelta which was created by Furiex Pharmaceuticals. MuDelta is a combo delta opioid receptor agonist(stimulates) and a mu receptor antagonist(blocks stimulation). The drug has similarities to another opioid receptor drug Naltrexone, however Naltrexone is purely a opioid receptor antagonist for the mu, kappa & to a small extent delta receptors. It does not have agonist properties and thus doesn’t stimulate any of the receptors.
Continue reading “Furiex’s New Irritable Bowel Syndrome Drug “MuDelta”” »
I posted a few days ago about Chelsey Macey who was suing Mission Organics, Natural Selection Foods & Dole Foods over E. Coli contaminated spinach which caused her to become deathly ill and later develop life altering Irritable Bowel Syndrome. Well the lawsuit is now settled out of court with the amount awarded to her sealed, so we don’t know exactly how much she was given, but the jury was already about to award $5 million in damages & had yet to decide on the award for pain & suffering. One would probably reason then that the the settlement was for over $5 million. Continue reading “Woman Settles Out of Court in Irritable Bowel Syndrome E. Coli Spinach Lawsuit” »
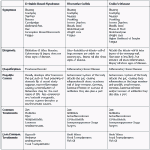
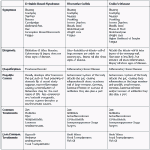
There seems to be some continual confusion about the differences between Irritable Bowel Syndrome & Inflammatory Bowel Diseases.
The main difference between the two is that Irritable Bowels Syndrome is a functional disorder, meaning there is little to no physical evidence of the disorder besides it’s symptoms. Inflammatory Bowel Diseases are not functional disorders and are diagnosable based off of physical evidence. Irritable Bowel Syndrome is usually much less severe than Inflammatory Bowel Diseases. Additionally “Inflammatory Bowel Disease” is not the actual name of a disease, but a classification for bowel diseases of an inflammatory nature. The two main Inflammatory Bowel Diseases are Ulcerative Colitis & Crohn’s Disease. They are not the same thing, though they have similar symptoms & treatments.
I made this handy chart below so people can get a better idea of the differences.
While searching the news today I saw a lot of outlets focusing in on a study recently released by the Statens Serum Institute(Denmark) about a possible link between antibiotics and Irritable Bowel Syndrome. Upon looking at the abstract and the title of the study I think we have a case once again of people mistaking Irritable Bowel Syndrome for Inflammatory Bowel Disease / Crohn’s Disease / Ulcerative Colitis. Continue reading “Study on Antibiotics is Related to Inflammatory Bowel Disease Not IBS” »
If you’ve made a new years resolution to lose weight this year & you have IBS, here’s some more motivation. A recent study(Reuters) by the Swedes at the University of Gothenburg shows that moderate to vigorous exercise for 20 – 60 minutes, 3 – 5 days per week can be helpful with Irritable Bowel Syndrome symptoms. The study showed 43% improvement for those in the exercise group, compared to 25% improvement for those who did not change their habits. Not earth shattering but it does hint that exercise can be helpful for Irritable Bowel Syndrome & of course exercise is usually good for you overall, something that most people probably don’t get enough of. Continue reading “Weight Loss Resolution Might Have Hidden IBS Benefits” »
A recent study review found that 12 out of 16 probiotic studies saw better outcomes when using multiple probiotic strains instead of just a single strain. These studies covered many different topics such as inflammatory bowel disorder, Helicobacter pylori, gut function & others.
I don’t find this terribly surprising as our digestive tract is teaming with all sorts bacterial flora. There is no jack of all trades probiotic that does everything for the digestive tract. There are also many different sub-strains of probiotics out there. If you go to the store you’ll probably see a lot of bottles labeled as being L. Acidophilus, however each company breeds it’s own strain(unless the companies outsourced from same lab) of L. Acidophilus so you might even get slightly different results depending on which brand you choose. There also may be a host of probiotic sub-strains we haven’t discovered yet. This is why something like fecal transplantation is interesting because it takes a working bacterial ecosystem and transplants it into someone who does not have one. It’s hard to slowly rebuild a healthy bacterial ecosystem with only a handful of bacteria, especially when we do not know which bacteria are most effective for each person & we may even be missing some.
I reported about a study on Rifaximin a few months ago. I was not that impressed by the results at that time. Well there has been a new study released on Rifaxmin showing pretty much the same unimpressive results. The facts are still that only about 11% saw benefit over placebo. That difference seems even more dubious what with the recent placebo study showing a similar level of efficacy. Who knows if the Rifaximin is really doing anything at all? Additionally patients are only tracked for 10-weeks, there is no information for what happens after that. It appears I am not alone in my concerns regarding the study. If you check out the comments on the study you’ll find there are a few doctors chiming in with their concerns:
“Here we go on another journey into a poorly supported area of new treatment…….this article barely shows a statistically signifincant difference, and certainly not a convincing one.” – MICHAEL ELIASTAM, MD
“This study is problematic in several ways, not least of which is the long list of companies involved, and somehow attached to the trial’s outcome.” – DAVID GLUCK, MD
“As a practicing gastroenterologist for 12 years as well as an IBS sufferer for almost 40, I realized long ago that we cannot treat IBS with a pill and that IBS is for life, and not for 10 weeks. I have been following Dr. Pimental’s studies for years, and I have yet to see anything last as long as the stress and psychological manipulation techniques that I and many others have been advocating for years.” – KIMBERLY CUSATO, MD
So buyer beware, Rifaximin may not be all it’s cracked up to be or what the hype my have you believe.
Chelsey Macey is the plaintiff of a lawsuit taking place in the Utah U.S. District Courts against Mission Organics, Natural Selection Foods & Dole Foods; who grew, packaged & distributed spinach that was contaminated with E. Coli in 2006. Macey’s infection with E. Coli was so severe that she was near death before recovering and developing chronic intestinal dysfunction which was diagnosed as Post-Infectious Irritable Bowel Syndrome. Continue reading “Lawsuit Claims E. Coli Caused Irritable Bowel Syndrome” »
A recently published study has some interesting insight on how the placebo effect may help Irritable Bowel Syndrome patients. A placebo in medical terms is essentially a “fake treatment” usually used to test the validity of drugs during testing. When a drug is being tested, patients are split into different control groups. One group is given a placebo(often a sugar pill) while the other is given the actual drug. The two groups are compared to see how effective the drug was versus the placebo. The interesting thing about the placebo is that in many cases people will see improvement in their symptoms during these studies even when they’re taking the placebo. This is called the “placebo effect”, where by the body responds to the notion that whatever they are being given is of benefit & somehow improves the persons condition despite the fact that there was nothing special in the pill. The actual reasons behind the placebo effect are still unknown, but it is quite interesting that the body has this response and it might prove beneficial for some people as this study shows. Continue reading “Some Irritable Bowel Syndrome Patients Respond to Placebo” »